STRENGTHENING HEALTH SYSTEM CAPACITY
FOR QUALITY IMPROVEMENT
Research Program 2 aims to embed quality improvement processes further within both clinical and non-clinical domains of comprehensive primary healthcare, for example strengthening service governance and workforce; engaging staff and management in quality improvement; and developing service-relevant best practice tools to address identified challenges, such as clinical follow-up.
Background
There is wide variation in key aspects of primary healthcare including preventive health, chronic illness, maternal and child health, and mental health and wellbeing care. The Engaging Stakeholders in Identifying Priority Evidence-Practice Gaps and Strategies for Improvement (ESP) highlighted these variations and identified key challenges (such as follow-up of abnormal clinical findings and workforce issues) and enablers to improvement (such as strong support for continuous quality improvement at all levels of the health system). Our work has already shown that steady improvements in primary healthcare quality and health outcomes are fostered by strong policy support and regional networks of continuous quality improvement facilitators. While key to enhancing effective quality improvement processes, there has been no rigorous investigation in the Aboriginal and Torres Strait Islander primary healthcare context of the influence of good quality practice-level facilitation that can: tailor continuous quality improvement support to individual services; build the continuous quality improvement capacity of multi-disciplinary teams; and provide continuous quality improvement tools, resources and networking. Furthermore, despite well-documented workforce issues in rural and remote Australia, little implementation research directly addressing such broader system issues has been conducted.
Program description
Research Program 2 aims to embed quality improvement processes further within both clinical and non-clinical domains of comprehensive primary healthcare by: i) examining how best to strengthen service governance and workforce; ii) exploring processes used by facilitators (in different contexts) to engage staff and management in quality improvement; and iii) developing service-relevant best practice tools to address identified challenges, such as clinical follow-up and improving efficiency in quality improvement processes.
Current projects
Implementation of quality improvement in Indigenous primary health care: Leveraging Effective Ambulatory Practices (LEAP)
CI Larkins & CI Matthews (co-leads), CI Bailie, CI Felton-Busch, AI Burgess, McBryde, AI Copley, Evans, Carlisle.
Summary:
Using case study methodology and ‘learning communities’, we are co-producing an understanding of contextual barriers faced by Indigenous PHC services that have struggled to reach improvement goals. We will co-produce a set of tailored tools and strategies to overcome barriers and apply these tools to other projects in this Research Program.
Resources:
Working It Out Together! Aboriginal and Torres Strait Islander led co-design for a strong and deadly health workforce
CI Larkins, CI Matthews, AI Walke, CI Felton-Busch, Taylor, AI Burgess, Tuala, AI Blackman, Carlisle.
Summary:
How do we embed Aboriginal and Torres Strait Islander perspectives into place-based/face-based planning and action for a stable and effective PHC workforce that engenders community trust in local care delivery?
Resources:
Promoting healthy ageing to reduce dementia risk in Aboriginal and Torres Strait Islander Communities
Strivens, Russell, Quigley, Hornby-Turner, Cadet-James, Howard.
Summary:
Dementia can be difficult for people and their family and caregivers. Studies show that Aboriginal and Torres Strait Islander peoples have a three to five times higher risk of dementia than non-Indigenous people, occurring at a younger age (45+). Health conditions such as diabetes, high blood pressure and heart disease, and lifestyle factors such as smoking and obesity increase the risk of dementia. The aim of this study is to work with Aboriginal health services to strengthen healthy ageing and dementia prevention services for their communities.
Resources:
Supporting Aboriginal people with cancer: development of training manual and training modules to support Aboriginal PHC services to deliver evidence-based care
Summary:
To evaluate the needs for cancer care training materials in ACCHOs in NSW and report on case studies of best practice cancer prevention and cancer care in NSW, to develop a training manual and training modules to support ACCHOs to deliver best practice cancer care to Aboriginal and Torres Strait Islander people, including QI programs, and to pilot and evaluate these.
Resources:
Seed-funded projects
Enhancing Point of Care testing and local workforce capacity in Aboriginal Communities through a continuous quality improvement approach
More info coming soon.
Dismantling systemic racism: educating health workforce through virtual understanding of Aboriginal and Torres Strait Islander experiences
More info coming soon.
Projects under development
Champions of Change: Strengthening facilitation for continuous quality improvement in Indigenous primary health care
Laycock, Feeney, CI Bailie, CI Passey, Carlisle, Clark, AI Copley, Patel, Harvey, Williams, AI Walke, Trask.
Summary:
The ‘Champions of Change’ project was initiated by the Northern Territory CQI Steering Committee and was developed through discussion with CQI support organisations and other CRE-STRIDE stakeholders. These groups identified a need to understand how CQI facilitators achieve engagement and enable impact in PHC settings, and how to improve the effectiveness and sustainability of facilitation practice for driving improvements in care.
Resources:
Completed projects
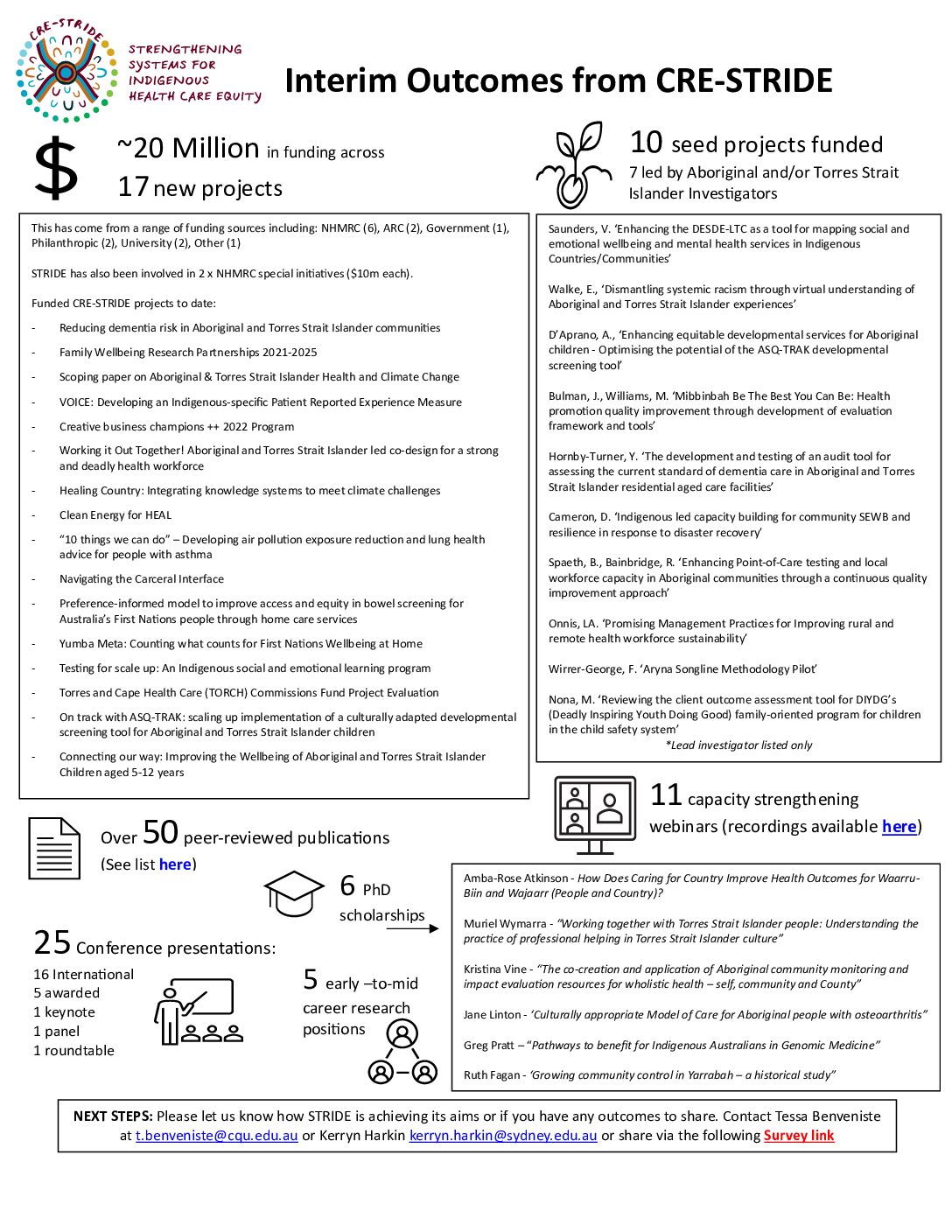
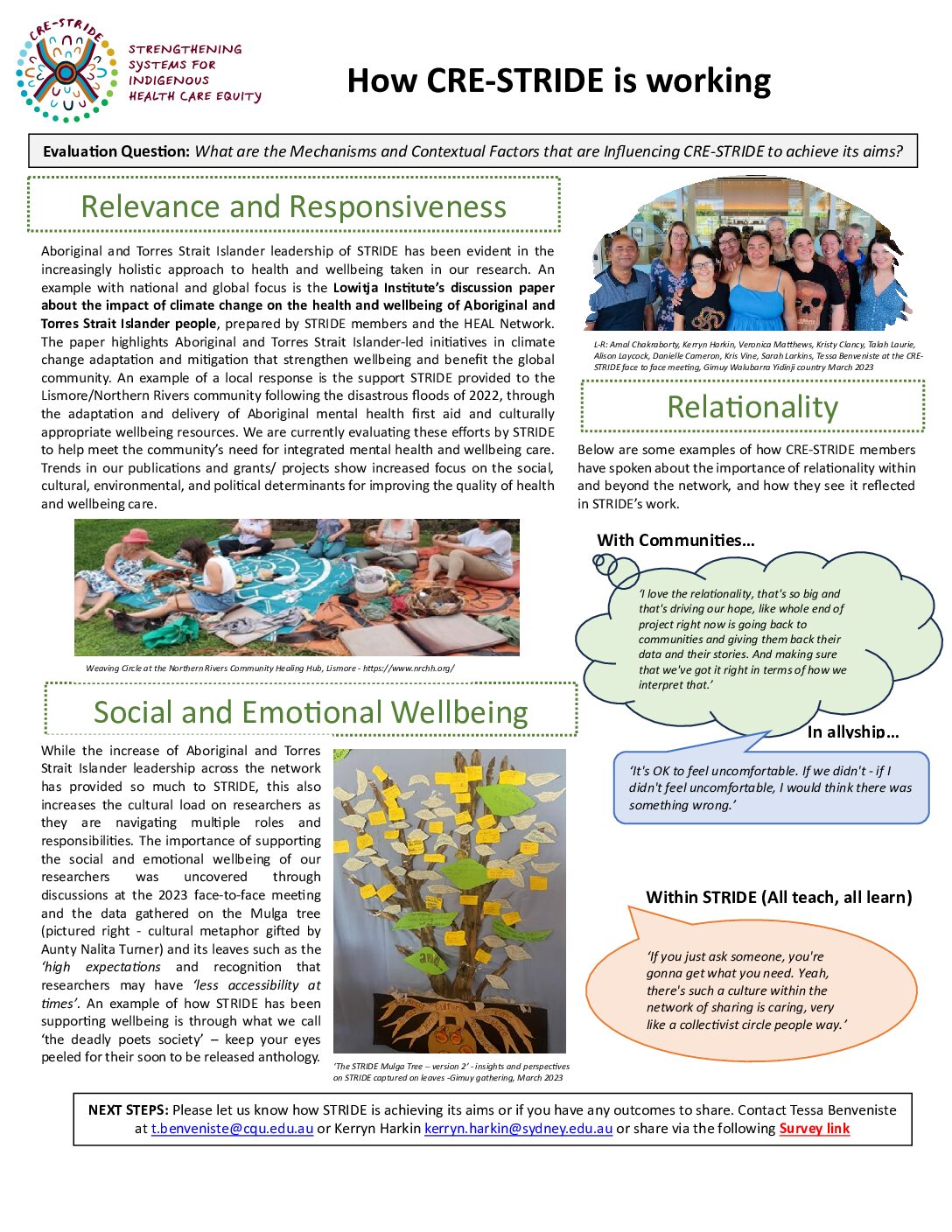
EVALUATION SUMMARIES (click on image to download)
THE STRIDE STORY (FILM) (click on image to view)
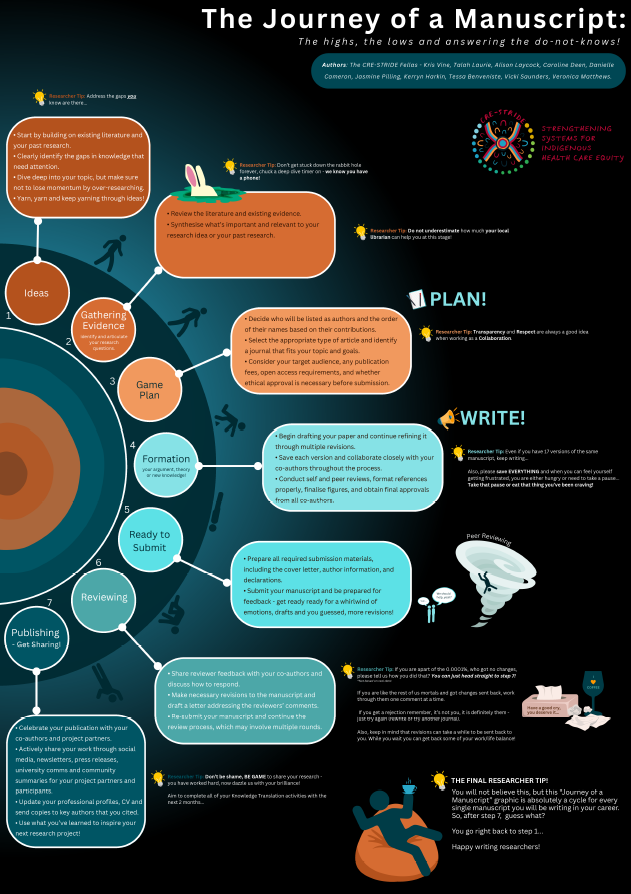
STRIDE FELLAS 'JOURNEY OF A MANUSCRIPT' (click on image to download)

VERONICA MATTHEWS (UCRH)
Veronica Matthews is from the Quandamooka community, Minjerribah (North Stradbroke Island) and a Wingara Mura Leadership Program Fellow at the University Centre for Rural Health, the University of Sydney. She has more than 15 years’ experience working in Indigenous health from program delivery and policy to research. She holds a PhD from the University of Queensland in environmental toxicology, has a Bachelor of Science and a Grad. Cert. (Epi) and is currently undertaking a Master of Applied Epidemiology through the Australian National University. Veronica has expertise in environmental health and Aboriginal and Torres Strait Islander health care systems research, with a particular focus on community engagement and resilience. Dr Matthews has advanced epidemiological skills, strong established networks and relationships in the Aboriginal and Torres Strait Islander health care sector and experience with facilitating grass-roots community-based participatory research.

SARAH LARKINS (JCU)
Professor Sarah Larkins is Dean of College of Medicine and Dentistry at James Cook University, and a part-time General Practitioner. She previously spent 12 years working in the community-controlled health sector as a GP. Sarah was awarded a Master of Public Health and Tropical Medicine in 2000 and a PhD in 2008 in Indigenous sexual and reproductive health. In 2009, she was selected from a global pool as a Brisbane Initiative scholar at Oxford University. Sarah is Co-Director of the Anton Breinl Research Centre for Health Systems Strengthening within Australian Institute of Tropical Health and Medicine. As well as strong links to the Queensland primary care, health services and Indigenous health community, she brings skills in research leadership and supervision, project management, research design, academic writing and dissemination and research translation. Her work responds to local and regional priorities and has a high degree of policy relevance and demonstrable uptake.

DR. SEAN TAYLOR (NT Govt)
Kerry Copley has worked for AMSANT since 2009, developing and supporting implementation of a CQI strategy for all Aboriginal primary health care services across the Northern Territory. She has been involved in developing the National CQI Framework and the ABCD (Audit and Best Practice for Chronic Disease) Partnership. Kerry was an Associate Investigator on the Lessons from the Best Research Project and is a Chief Investigator on the LEAP (Leveraging Effective Ambulatory Practices) Research Project. She has substantial experience in primary health care management and CQI roles. Prior to AMSANT, Kerry was Deputy CEO for the Divisions of General Practice in the Northern Territory.

KERRY COPLEY
Kerry Copley has worked for AMSANT since 2009, developing and supporting implementation of a CQI strategy for all Aboriginal primary health care services across the Northern Territory. She has been involved in developing the National CQI Framework and the ABCD (Audit and Best Practice for Chronic Disease) Partnership. Kerry was an Associate Investigator on the Lessons from the Best Research Project and is a Chief Investigator on the LEAP (Leveraging Effective Ambulatory Practices) Research Project. She has substantial experience in primary health care management and CQI roles. Prior to AMSANT, Kerry was Deputy CEO for the Divisions of General Practice in the Northern Territory.